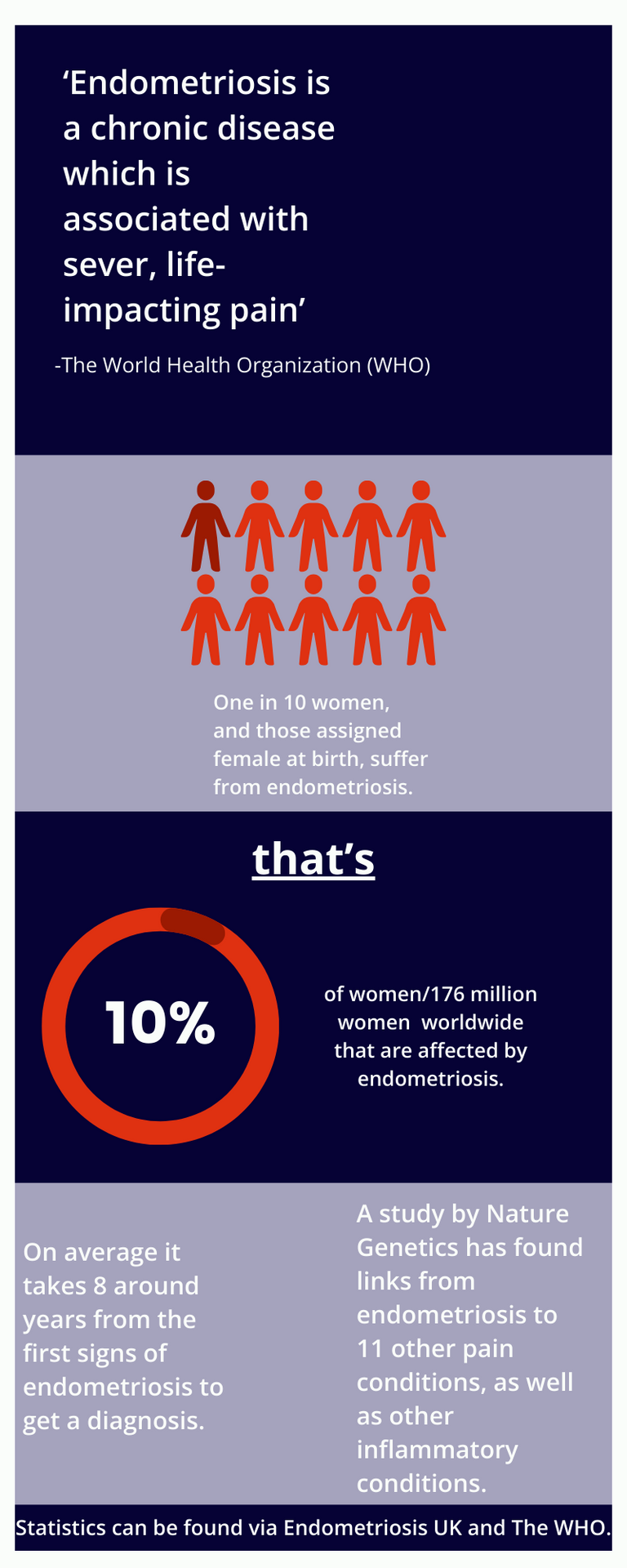
According to Endometriosis UK, 1 in 10 women and those assigned female at birth, who are at reproductive age, suffer from endometriosis. Endometriosis also affects 176 million women worldwide, equating to a staggering 10% of women. Yet, there is still a big misunderstanding around the condition and many think it just causes painful periods. So, with so many women living with endometriosis, what actually is it?
What is it?
The World Health Organization (WHO) states endometriosis is a chronic disease which is associated with severe, life-impacting pain during periods, sexual intercourse, bowel movements and/or urination, chronic pelvic pain, abdominal bloating, nausea, fatigue, and sometimes depression, anxiety, and infertility.
When a person has endometriosis, tissue similar to the lining of the uterus, grows elsewhere in the body. Each month, the tissue acts as it would do in the uterus and tries to leave the body as a period, but unlike from inside the uterus, the blood has nowhere to escape from. This causes severe pain and can cause issues with fertility. Endometriosis can start from a person’s first period, right up until menopause, but the impact can be felt throughout their whole life.
The cause for endometriosis is unknown and there is no way to prevent it. Currently, there is no cure and treatment is aimed at controlling the symptoms. Treatment for endometriosis usually results in surgery to cut away endometriosis tissue, and in some severe cases part, or all of the organs affected are removed.
The WHO states that early diagnosis and effective treatment of endometriosis is important to enable the management of symptoms. However, according to Endometriosis UK, on average it takes around 8 years from the first signs to get a diagnosis. This is because the symptoms can vary considerably from person to person, and there are many other conditions which can cause similar symptoms. However, this still means that sadly, many women suffer with the effects of endometriosis for years without treatment and support to help manage their often debilitating pain.
Lived experiences
We spoke to two friends, Lucy and Johanna, who are both women in their late twenties with varying experiences of endometriosis. We asked them to tell us about their journeys to diagnosis and treatment.

Lucy's Story
‘Hi, my name is Lucy. I first knew something was wrong back in college when my periods were so painful that I would be taking as much pain relief as I could, whilst still suffering with extreme cramps and heavy bleeding. I was referred for a scan in 2017 where I was told I had a 5cm haemorrhagic cyst on my ovary and discharged from care with no help for my symptoms.
Four years later in November 2021, with no improvement in my pain or symptoms, I pushed for another referral and finally got an appointment for another scan. Following the scan, I was told my cyst remained and it was going to be monitored over 6months for any changes. I was also advised to go on the contraceptive pill to try and help symptoms.
After my 6 month review I was finally placed on the waiting list for a laparoscopic excision of what they suspected was endometriosis. It took me a further 12 months from signing the consent form to the operation date. Unfortunately, when I woke up from my operation, I was told that I had stage 4 endometriosis, and that all my pelvic organs were stuck together with adhesions. It was specifically worse in between my vagina and rectum, and as they didn’t want to cause any permanent damage to my bowel, they referred me for an MRI to see how deep the lesions were before operating on them.
The results of my MRI and pathology have shown that the endometriosis is deep within my bowel wall, so now I must have bowel surgery to avoid any serious complications like bowel obstruction. I am now on a further waiting list which is 12- 18 months long. Before having my surgery, I was so nervous that they would not find anything, and I would be left wondering what was wrong with me and I’d be back to square one. I don’t think there are enough resources or awareness for people with endometriosis as I’ve often been dismissed and told it is ‘just a period’. I find this so disappointing as I now must have a bigger operation because I was not listened to sooner. I would advise anyone who is worried about their symptoms to get referred and do not give up!’
Johanna's Story
'Hello, my name is Johanna, and I am 108 days post-op from my diagnostic laparoscopy. Let's rewind to the beginning of where my symptoms began in 2020, I had my little girl in the August. After that, I began noticing symptoms that included heavy bleeding and very painful periods. I was told numerous times that this is normal after having a child, and something I should get used to. I got advised by my GP that contraception would help reduce the symptoms, so I took their advice and got the Mirena coil. My symptoms persisted and even worsened; I had non-stop bleeding every day for nine months. I eventually got the coil removed and being put off by the experience I refused any other contraception. Being a first-time mum and experiencing these symptoms constantly was scary, so I repeatedly went to the doctors. In September 2021 I finally got a referral through to see a gynaecologist. The waiting time for this felt like forever.
January 2022, and my first meeting with the gynaecologist finally came. I felt heard for once and understood. Nothing prepares you for pain like I’d experienced, and only you know your body and when something isn't right. Without the support from my amazing family, friends, and partner, I can't imagine the state I would really be in. After many visits to the GP, A&E and the Gynaecology Assessment Unit, I finally have an answer and don't feel like I am losing myself anymore. My symptoms had taken such a toll on my mental and physical health for years.
Post-op things have felt a lot better, with pain being more tolerable. I am lucky enough to say that all the endometriosis tissue has been successfully removed and I continue to stay positive for a healthier and pain free life. I am told there is a chance that the tissue can grow back, but I am trying to stay positive. Don't be afraid to stand up for yourself in situations when you don't feel heard, you are not alone.’
Some things that Johanna and Lucy say they use to help manage their pain and symptoms are painkillers, and the use of a TENS Machine. TENS machines can fit to the outer area where you are experiencing pain, such as the pelvic area, and small electrical impulses are sent to the area to interrupt the pain signals which go to the brain. Johanna has said this has been especially helpful when she is experiencing a flare up. However, these things only help to manage the pain and mask the symptoms, and it is advised to speak to your GP and push for a referral if you are experiencing any of the symptoms mentioned above.
Awareness around endometriosis and research into the condition has improved in recent years. In March 2023, the largest ever study on the genetics of endometriosis was published in Nature Genetics, finding genetic links to 11 other pain conditions as well as other inflammatory conditions. However, the awareness and understanding of the condition does still have a way to go so that the average diagnosis time of 8 years can be minimised and women can be treated quicker, without being dismissed with just a painful period.
We hope you have found this article helpful and informative. It’s important to note that this article has not been written by a health care professional and if you are experiencing pain or any of the symptoms above, please do speak to your GP.
To view the sources listed in this article please click on the bold and underlined text. You can also find them listed below.